|
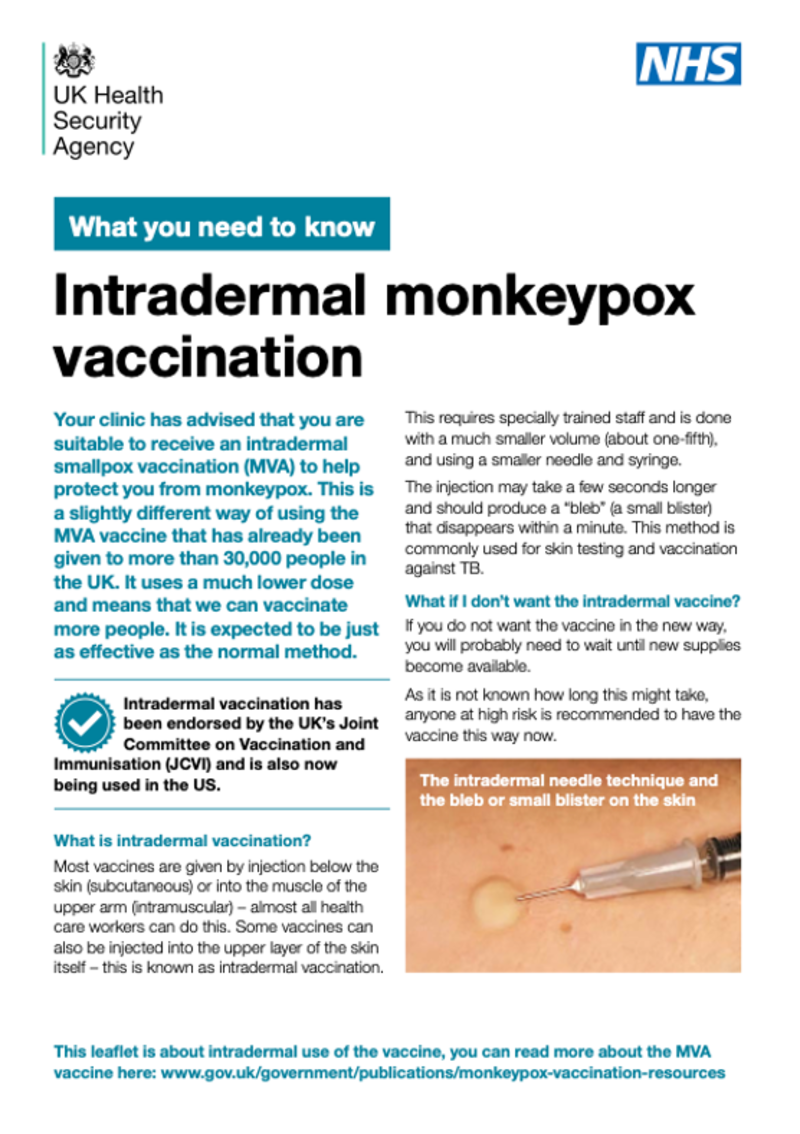
Mpox is an infectious disease caused by the monkeypox virus. This can cause a painful skin rash, fever, headache, enlarged lymph nodes, as well as muscle aches, along with other symptoms. Most people fully recover. But some people may become very ill and the disease can be fatal. Outbreaks have most commonly occurred in East, West or Central Africa. But mpox has been found in many other countries globally, including the UK. This is particularly the case since 2022. There are currently two types (clades) of mpox circulating; clade 1 and clade 2. Clade 2 is behind the global outbreak that began in 2022. Although this outbreak has declined substantially since its peak, cases are still around. And the World Health Organization (WHO) is concerned about the emergence of a new version of clade 1 (clade 1b) as it appears to cause more severe disease and a higher death rate than other clades. So far, clade 1b mpox has been detected in the DRC and a few surrounding countries. Global cases have also been detected, with a handful of cases, who all share a household, being detected in London. In August 2024, the WHO declared the emergence of this new mpox clade a Public Health Emergency of International Concern (PHEIC) to enable an international response to prevent both this new mpox outbreak and existing outbreaks. Please go to our mpox infectious disease information for more detail. Vaccines are available for people recommended vaccination (see section below). The mpox virus is related to the smallpox virus, which was eradicated globally at the end of the 1970s because of the success of that vaccination programme. Because of the similarities between the two viruses, vaccines that were developed to prevent smallpox are being used against mpox. In the UK, the Modified Vaccinia Ankara – Bavarian Nordic (MVA-BN) vaccine is offered to people considered at high risk. Two doses are needed for the best protection. MVA-BN is sold under two trade names; Imvanex in the UK and Jynneos in the US. The MVA vaccine uses a much weakened form (attenuated) of a pox virus called vaccinia to induce an immune response. Globally, two other vaccines are recommended by the WHO – LC16 and ACAM2000. These also use greatly weakened versions of the vaccinia virus. However, these aren’t recommended for some people, such as those who are immunocompromised or pregnant. The mpox vaccine can be given either before exposure to the virus, or after an exposure has taken place. The vaccine is less effective post-exposure and rarely given. Mpox - here's what you need to know Mpox - here's what you need to know
https://www.youtube.com/embed/uBi8Zn7Z63o?wmode=opaque&controls=&rel=0
|