|
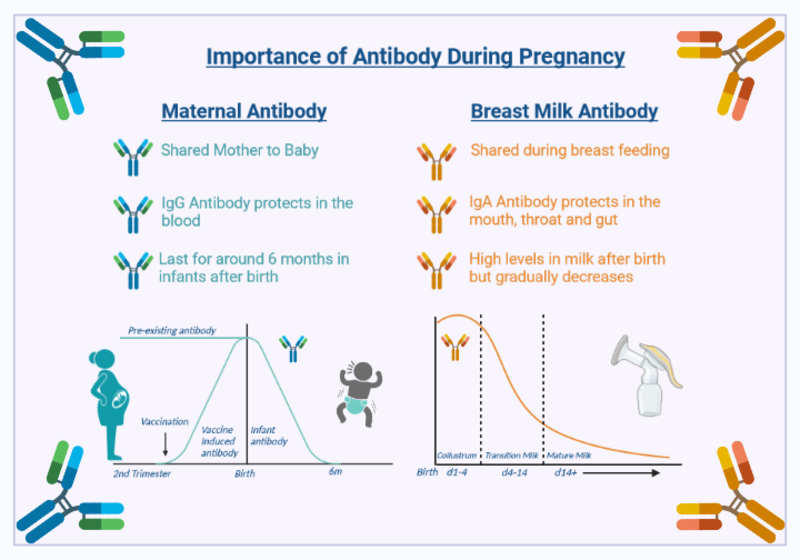
Three vaccines are currently recommended for pregnant individuals in the UK, these are: 1. The Flu vaccine The risk from serious influenza is especially high in pregnancy. Death rates from flu are higher among pregnant individuals than among people who are not pregnant. Flu in the mother is also a risk to the baby, but vaccination protects pregnant people and their babies from these effects. In the 2020-21 flu season, over 43% of pregnant people in England (more than 264,000 people) received the flu vaccine. 2. The Pertussis (whooping cough) vaccine Almost all deaths from whooping cough occur in young babies before they have had a chance to be vaccinated. Babies can be protected by vaccinating the mother during pregnancy. In 2020-21, over 67% of pregnant people in England received the whooping cough vaccine. Pregnant people are more at risk of becoming seriously ill from COVID-19 and are at an increased risk of complications such as preterm labour and stillbirth. Almost all pregnant individuals hospitalised or admitted to intensive care with COVID-19 between May-October 2021 were unvaccinated (96%). COVID-19 vaccines are safe and effective in pregnant individuals and protect both mother and child. |