How well does the vaccine work?
A recent Cochrane review of 124 studies assessing vaccine effectiveness showed that two doses of MMR vaccine were 96% effective in preventing measles, and one dose was 95% effective in preventing measles.
Two doses of MMR vaccine are also around 86% effective against mumps, and 89% effective against rubella.
Public Health England estimates that around 20 million measles cases and 4,500 deaths have been prevented in the UK since a measles vaccine was introduced in 1968.
In addition, they estimate that rubella vaccination has prevented around 1.4 million cases of rubella and 1,300 cases of birth defects and averted 25,000 terminations.
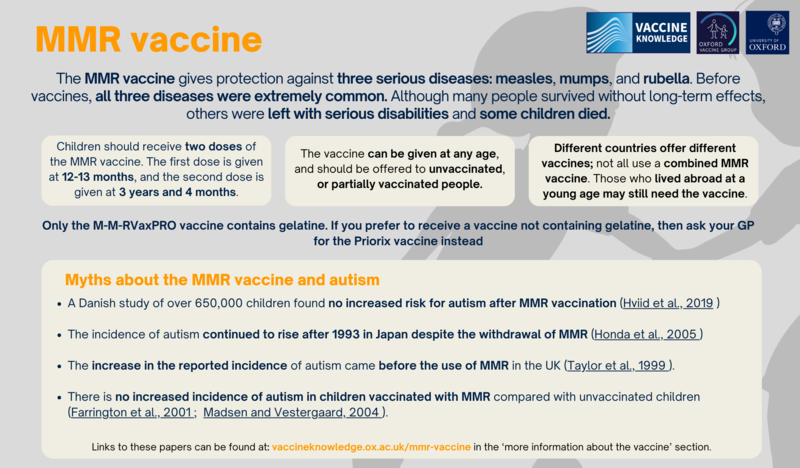
Myths about the MMR vaccine and autism
There is no evidence of any link between the MMR vaccine and autism. Autism is a developmental disorder which is usually diagnosed in preschool children. The original research which suggested a link has now been discredited.
The National Autistic Society in the UK has issued a statement saying that ‘there is no link between autism and the MMR vaccine’.
Below is a list of studies and their findings. Click on the links to view the abstracts (summaries) of the scientific papers:
- A Danish study of over 650,000 children found no increased risk for autism after MMR vaccination (Hviid et al., 2019 )
- An analysis of studies involving over 1 million children found no relationship between vaccination and autism. There was no evidence of a link between the MMR vaccine and autism development in children, and the study also found no evidence of a link between thiomersal and autism development (Taylor et al., 2014 ).
- There is no increased incidence of autism in children vaccinated with MMR compared with unvaccinated children (Farrington et al., 2001 ; Madsen and Vestergaard, 2004 ).
- There is no clustering of the onset of symptoms of autism in the period following MMR vaccination (Taylor et al., 1999 ; Mäkelä et al., 2002 ).
- The increase in the reported incidence of autism preceded the use of MMR in the UK (Taylor et al., 1999 ).
- The incidence of autism continued to rise after 1993 in Japan despite withdrawal of MMR (Honda et al., 2005 )
- There is no correlation between the rate of autism and MMR vaccine coverage in either the UK (Kaye et al., 2001 ) or the USA (Dales et al., 2001 )
- There is no difference between the proportion of children with a regressive form of autism (i.e. who appear to develop normally but then lose speech and social skills between around 15 and 30 months) who develop autism having had MMR compared with those who develop autism without vaccination (Fombonne and Chakrabarti, 2001 ; Taylor et al., 2002 ).
- There is no difference between the proportion of children developing autism having had MMR who have associated bowel symptoms compared with those who develop autism without vaccination (Fombonne and Chakrabarti, 2001 ; Taylor et al., 2002 )
- No vaccine virus can be detected in children with autism using the most sensitive methods available (Afzal et al., 2006 ; D’Souza et al., 2006 ).
Planned changes to the MMR schedule
The Joint Committee on Vaccination and Immunisation (JCVI) advised that the second dose of the MMR vaccine, usually given at 3 years 4 months, should be brought forward to 18 months of age.
The main purpose of bringing the second dose forward is to improve coverage of the second dose, and further reduce the likeliness of measles outbreaks.
In some areas of London, where the second dose of the MMR vaccine has previously been brought forward in response to local measles outbreaks, second dose coverage increased by an average of 3.3 percentage points.
This earlier visit would create a new immunisation visit, but the probable benefit of increasing coverage in MMR justifies the JCVI’s decision. Furthermore, due to the recommended changes to the other vaccine schedules, an additional dose of Hib-containing multivalent vaccine (such as the DTaP/IPV/Hib/HepB which is also given earlier in infancy) should also be given at 18 months.
These changes will occur once the current stock of Menitorix, the current Hib-containing vaccine, runs out.
Read more in the Joint Committee on Vaccination and Immunisation (JCVI) statement on changes to the childhood immunisation schedule here.