|
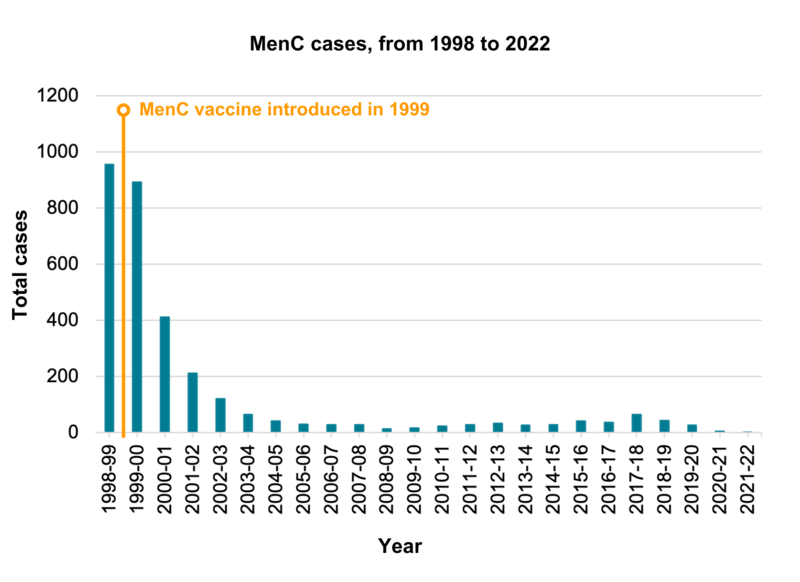
The single MenC vaccine was in the routine UK immunisation schedule from 1999 until July 2016. This vaccine gives protection against meningococcal disease, a major cause of meningitis, that is caused by group CNeisseria meningitidis bacteria. Babies and children are still protected against MenC disease through the Hib/MenC vaccine given at a year of ageand the MenACWY vaccine given to teenagers, but the single MenC vaccine is no longer routinely used in the UK. The MenC vaccination programme was introduced in the UK in 1999 and quickly led to a dramatic fall in the number of cases of MenC disease. Meningococcal bacteria are commonly carried in the back of the throat and passed around from person to person in an unvaccinated population. The vaccine prevents the carriage (the harbouring of) MenC bacteria in the back of the throat which means that even people who are not vaccinated are protected by herd immunity. Recently, the Joint Committee on Vaccination and Immunisation (JCVI) was notified that Menitorix, the Hib/MenC currently used in the UK, will be discontinued by the manufacturer for commercial reasons. Based on the demonstrated decline of invasive meningococcal A, C, W and Y disease in the UK, primarily through vaccination programmes, the inclusion of a MenC-containing vaccine (such as MenACWY) in the infant schedule will not continue once stocks of Hib-MenC run out. See below for more information. Currently, there are almost no cases of MenC disease in infants or young children in the UK. Before vaccination, there were nearly 1000 cases a year and 70-80 deaths a year – Public Health England and Health Protection Agency Archive. MenC vaccines licensed in the UK included NeisVac-C and Menjugate. |