|
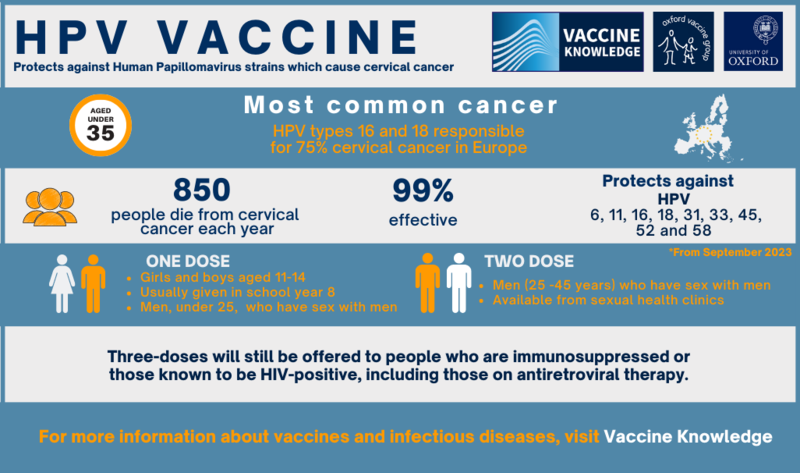
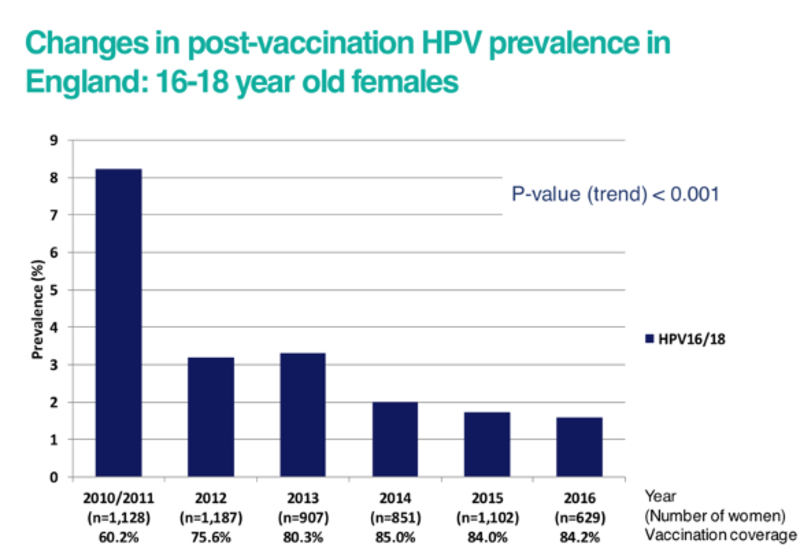
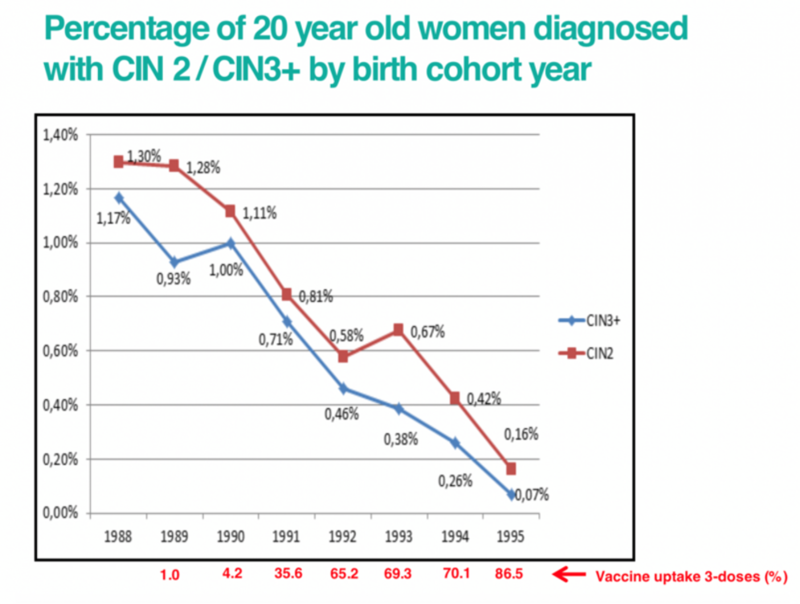
Human papillomavirus (HPV) is a family of viruses which cause a range of serious diseases including cervical cancer and mouth cancer. There are approximately 100 types of HPV. Around 40 types infect the genital tract and are associated with genital warts and various types of cancer in men and women. Over 99% of cervical cancers are caused by HPV infection. Two high-risk types, HPV 16 and HPV 18, are responsible for nearly 75% of all cervical cancers in Europe. Cervical cancer is the most common cancer among women who are 15 to 34 years old. Unlike most cancers, it is mainly a disease of the young, with 62% of cases occurring in women who are less than 50 years old. Worldwide, cervical cancer is the fourth most frequent cancer in women with an estimated 604,000 new cases and 342,000 deaths from cervical cancer in 2020. About 90% of these occur in low- and middle-income countries. However, studies looking at the percentage of women diagnosed with cervical abnormalities have shown a marked reduction since the introduction of the HPV vaccination programme. See more information below. Before vaccination started in 2009, HPV was the most common sexually transmitted infection (STI) in the UK. |